Dental Implants, also known as endosseous implants, are titanium replacements for missing teeth which are surgically implanted into the jaw bone.
Prosthetic teeth (also known as crowns) are firmly attached to the dental implant which is secured into the jaw, and is not removable. Dental implants are considered the gold standard in the replacement of missing teeth, providing a better, more comfortable and attractive solution than traditional dentures. Most people with dental implants describe the feel is much closer to natural teeth than with dentures.
Adelaide MaxFax – The Team Approach to Dental Implant Treatment
Adelaide MaxFax firmly believes in a Team Approach when managing patients requiring oral reconstruction with dental implants.
We strongly believe the best long term, functional and aesthetic outcomes are achieved when patients receive care from a multi-disciplinary team. This is evidence based and has been confirmed by numerous studies in both the medical and dental academic literature.
The best team to complete your care should be your dentist and/or a specialist prosthodontist, an oral and maxillofacial surgeon, and a dental technician. All have their specific skill sets which, when combined, give the patient the best possible results.
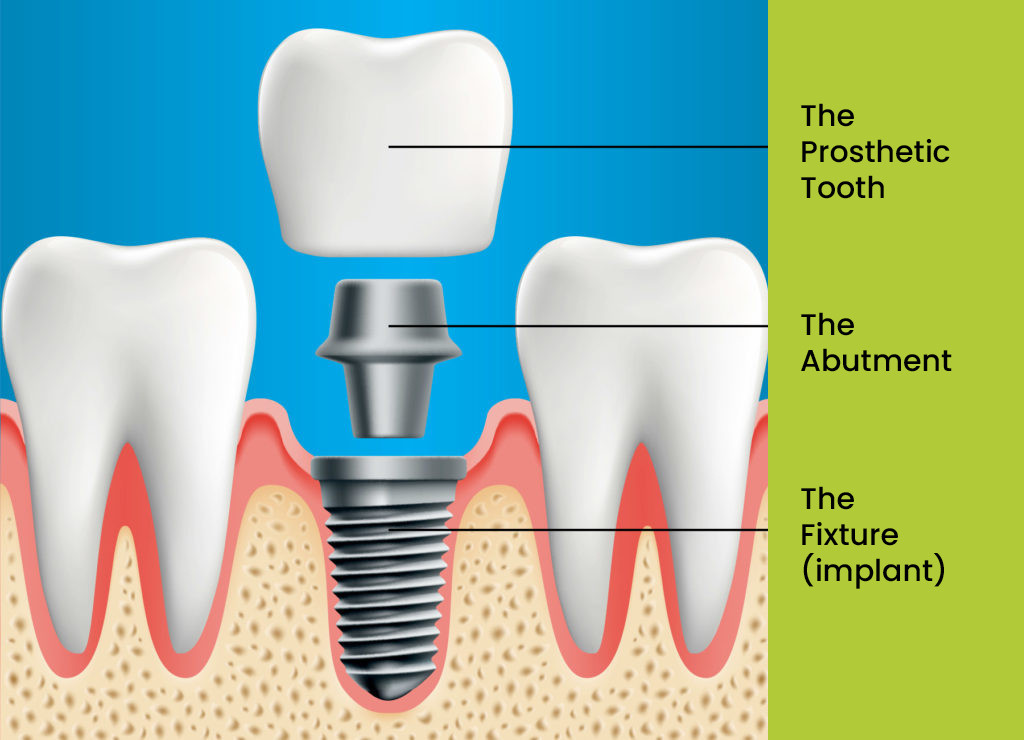
A dental implant consists of three parts:
The Fixture (made of titanium) is surgically placed in the jawbone below the gum.
The Abutment (made of titanium), emerges through the gum, and is a separate component. The abutment is attached to the fixture which acts as the foundation for the prosthetic tooth (prosthesis).
The Prosthetic Tooth (made of white, tooth coloured ceramic) or teeth (prosthesis).
There are several types of dental prosthesis:
-
A single prosthetic tooth (implant retained crown)
-
Several prosthetic teeth in a row (implant retained bridge)
-
A full set of prosthetic teeth, held in place by several implants (implant retained denture)
Implant supported crown
Implant supported bridge
“All on X” concept, Implant supported denture
Your dentist can refer you to Adelaide MaxFax to discuss the suitability of implant treatment, and the type of treatment that will best suit your individual needs. Dr Khouri will work with your dentist throughout the process to help you achieve an excellent result.
For more complex implant rehabilitation including full mouth dental implant reconstruction, Dr Khouri works closely with specialist prosthodontists to achieve excellent results.
The Adelaide MaxFax team is here to assist you at all times. Should you have any questions or concerns regarding an upcoming procedure, please reach out to us without hesitation.
76 Kensington Road, Rose Park, SA 5067
Phone: (08) 8332 1566
Fax: (08) 8364 2890
Email: [email protected]
Opening hours:
Monday – Friday 9am to 5pm
Parking and access
Patient parking is conveniently located behind the surgery, accessible via Winchester Lane. The main entrance for patients is situated at the front of the building, while disabled access is available behind the surgery.